Varicose Veins
What Are Varicose Veins?
Varicose veins are swollen, bulging veins that you can see just under the surface of your skin, most commonly found in the legs and feet. Varicose veins can either be buried deep within the body or close to the skin’s surface and visible, often called spider veins. Although both have the potential to cause discomfort, proper treatment through minimally invasive procedures with the dedicated vascular specialists at Pedes Orange County can provide our patients with long-term relief.
Symptoms of Varicose Veins
Varicose veins are twisted, enlarged veins that can cause discomfort and cosmetic concerns. They often present with a variety of symptoms that may affect daily activities and overall well-being.
Common varicose vein symptoms include:
- Aching or heavy sensation in the legs
- Burning, throbbing, or muscle cramping
- Swelling in the lower legs
- Itching around one or more veins
- Skin discoloration around the affected veins

Causes of Varicose Veins
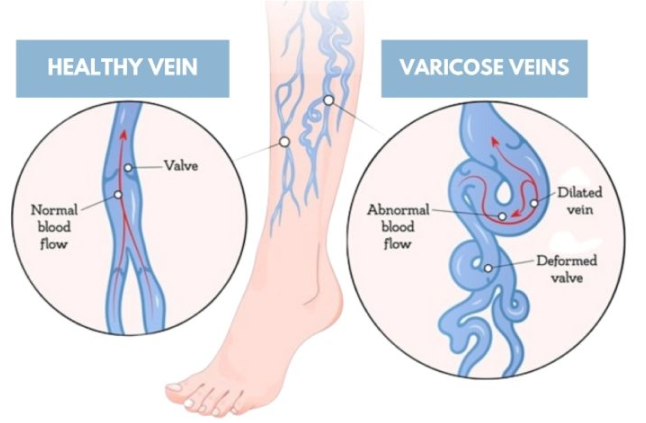
Varicose veins are most commonly caused by valves within the veins malfunctioning. Rather than
allowing blood to flow smoothly back to the heart, damaged or worn valves allow the blood to backflow and pool within the veins. This backflow causes the signature swelling and enlargement that we see in varicose veins.
While damaged or missing valves within the veins are the most common cause of varicose veins, other less common causes include:
- Inflammation in the veins (phlebitis).
- Congenital abnormalities within the veins.
- Blood clots or other conditions that may obstruct blood flow to the heart.
Common risk factors associated with the development of varicose veins include older age, pregnancy, sitting or standing for long periods of time, obesity, and genetic factors.
Varicose Veins Complications
Although not very common, there are some complications that may arise as a result of varicose veins.
Varicose veins have the potential to form painful wounds that form on the skin near the affected veins on the legs and ankles. If you see discolored spots near your varicose veins and suspect non-healing ulcers<link DD> are forming, we encourage you to seek medical attention from our vascular specialists immediately.
Various studies show that women are more susceptible to varicose veins than men are. Hormonal changes during pregnancy or before the menstrual period cause the veins’ walls to relaWhen blood pools in the veins, the veins become painful and swell, increasing the risk of blood clots. If you experience chronic inflammation in the veins in your legs, seek medical attention from our vascular doctors immediately. Blood clots that are untreated may move up the veins and have the potential to cause a stroke.x, leading to blood backflow. Additionally, hormone treatment such as birth control pills can also increase your susceptibility to this condition.
When the pressure builds up in the veins close to the skin, they eventually burst, causing minor bleeding.
While the skin breakout may be minor, seeking medical attention is crucial to prevent further complications.

Diagnosing Varicose Veins
Diagnosing varicose veins is typically a simple process, as the veins are often visible on the skin’s surface.
However, your diagnostic process may include a physical examination and ultrasound imaging to determine the extent of your condition and to view how the veins are functioning deep within the body. Our dedicated vascular doctors may also ask you to describe your symptoms, including any aching or pain you feel in your affected limbs.

Treatments for Varicose Veins
There are many treatments for varicose veins available, from nonsurgical medical treatments to minimally invasive procedures. Oftentimes, patients turn to endovenous laser ablation or Varithena®, an injectable microfoam treatment, as nonsurgical solutions. Some patients may also turn to phlebectomy or vein stripping, which tie off or remove the veins entirely to address their discomfort.
At Pedes Orange County, we offer a range of effective, nonsurgical treatments to address both the
discomfort and appearance of varicose veins. Our range of medical treatments and minimally invasive procedures includes:
- VenaSeal™
- Radiofrequency ablation (FRA)
- Ultrasound-guided sclerotherapy
- Microphlebectomy
In addition, we also offer Cutera Excel® V Laser treatments and sclerotherapy treatments to address the unwanted appearance of varicose veins. We encourage you to learn more about the varicose vein treatments offered by the specialists at Pedes Orange County below.
Contact Us Today


Our Vascular Disease Physicians
The physicians at Pedes Orange County devote their lives to saving limbs and minimizing pain. Our conveniently located, state-of-the-art facility is designed for your comfort and utilizes cutting-edge technology to provide minimally invasive treatments. Our vascular specialists are board-certified and some of the best in Southern California. Personable staff members make every visit a positive experience, with short wait times and an efficient, streamlined process that ensures you leave feeling educated and confident that you are in good hands.

J. Joseph Hewett, M.D.
Vascular Specialist

Neil K. Goldstein, M.D.
Vascular Specialist

Derrick Tran, MD
Vascular Specialist

Mohammad Jaber, M.D.
Vascular Specialist
Why Chose Pedes Orange County?
A spider vein looks very different from a varicose vein, and generally, they don’t affect you like varicose veins, but they can be just as severe as varicose veins when they are in groups or clumps. Preventing this condition is possible through self-care and minor lifestyle adjustments. It’s vital to be proactive if your family has a history of the condition. Give us a call and talk to one of our specialists.
What to Expect from Your Visit to Pedes

Ultrasound
Advanced ultrasound-guided examination techniques will be used to visualize the veins, arteries, or both, in your legs. This is often used in the diagnostic process to detect the presence and extent of disease.

Consult
Once we review the results of your diagnostic tests, our physicians will collaborate with you to develop a personalized treatment plan, ensuring the best course of treatment for your specific condition.

Treatment
Your treatment plan will be personalized to you and your individual needs. At Pedes, we specialize in minimally invasive procedures and nonsurgical treatments, all of which are performed by our dedicated vascular physicians within the comfort of our state-of-the-art facility.

Follow up
We ensure our patients receive continuous care and support with regular follow-up visits. Each follow-up visit is scheduled at the time of your in-office appointment. Should you have a concern between
appointments, we encourage you to call our office and get scheduled at any time.







