Pelvic Venous Disease
Most people know varicose veins mostly affect the feet and legs
But varicose veins can also occur in the pelvis causing chronic pelvic pain in women; this condition is known as Pelvic Venous Congestion Syndrome (PVCs) or ovarian vein reflux. Herein is a look at the condition, the risk factors, causes, symptoms, and treatment options. Read on to find out more.
What is Pelvic Venous Disease?
Pelvic venous disease encompasses conditions like pelvic venous congestion syndrome (PVCS) and May-
Thurner syndrome, both of which involve abnormal blood flow and vein enlargement in the pelvic region. PVCS is characterized by chronic pelvic pain due to varicose veins in the pelvis, while May- Thurner syndrome involves compression of the iliac vein, leading to leg swelling and discomfort.
These conditions are often underdiagnosed, resulting in prolonged suffering for many patients. At Pedes Orange County, we provide comprehensive diagnostic services and personalized care to effectively manage and treat pelvic venous disease, helping patients regain their quality of life and well-being.
Symptoms of Pelvic Venous Congestion Syndrome (PVCS) include:
Pelvic venous congestion syndrome (PVCS) is a condition caused by varicose veins in the pelvic region, leading to chronic pelvic pain. This pain is often dull and aching, exacerbated by prolonged standing or after engaging in physical activities. PVCS can significantly impact daily life and overall comfort but is manageable with proper diagnosis and treatment.
Symptoms of Pelvic Venous Congestion Syndrome (PVCS) include:
- Chronic pelvic pain lasting six months or longer
- Pain that worsens with standing or physical activity
- A feeling of fullness or pressure in the pelvis
- Visible varicose veins in the buttocks, thighs, or vaginal area
- Painful menstrual periods
Oftentimes, women who experience the symptoms of PVCS are directed to their gynecologist’s office for further testing. However, it takes the skill and expertise of a vascular specialist to provide proper care for this condition. If you are experiencing two or more of the above PVCS symptoms, we encourage you to call our office right away to schedule your appointment.
Pelvic venous congestion syndrome (PVCS) is primarily caused by malfunctioning valves in the pelvic veins, leading to blood pooling and vein enlargement.
The most common causes of PVCS include:
- Malfunctioning or weakened vein valves
- Hormonal changes during pregnancy
- Anatomical variations or abnormalities in pelvic veins
Increased pressure on pelvic veins due to prolonged standing or heavy lifting
There are many factors that may heighten a patient’s risk of developing PVCS, including:
- Pregnancy, due to increased blood flow and hormonal changes
- Multiple pregnancies, which can exacerbate vein stress and valve dysfunction
- Family history of varicose veins or venous disorders
- Hormonal imbalances, particularly elevated estrogen levels
- Prolonged periods of standing or heavy lifting
- Pelvic surgery or trauma that may affect vein function
While many women may experience pelvic pain at some point in their lives, it’s not always caused by the congestion of blood vessels or veins. For this reason, it’s often difficult for doctors to diagnose PVCS.
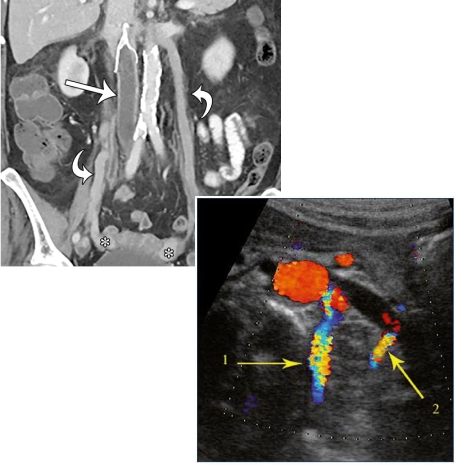
The vascular specialists at Pedes Orange County use a combination of advanced imaging techniques to accurately diagnose pelvic venous disease including pelvic venous congestion syndrome in our patients. These imaging techniques include:
- Pelvic or abdominal ultrasound
- Pelvic or abdominal CT and MRI scans
- Pelvic venography using X-ray imaging
At Pedes Orange County, we offer ovarian vein embolization as an effective treatment for pelvic venous congestion syndrome (PVCS). This minimally invasive procedure targets and seals the problematic veins using tiny metal coils, medical glue, or foam, alleviating pain and improving blood flow. Our dedicated team ensures a compassionate and personalized approach to care, helping patients achieve lasting relief and enhanced quality of life.
May-Thurner Syndrome
May-Thurner Syndrome is a pelvic venous condition where the right iliac artery compresses the left iliac vein, stopping normal blood flow from the legs to the heart. This compression can lead to symptoms such as leg pain, swelling, and an increased risk of deep vein thrombosis (DVT). Early diagnosis and treatment are crucial to managing this condition effectively and preventing complications.
Symptoms of May-Thurner Syndrome include:
- Persistent leg pain, often in the left leg
- Swelling in the legs, especially after prolonged periods of standing or sitting
- A feeling of heaviness or fatigue in the affected leg
- Visible varicose veins in the leg or pelvic area
- Skin discoloration or ulcers on the lower extremities
While May-Thurner Syndrome commonly affects women, it is important to note that men may also develop the condition. If you suspect your male loved one may have May-Thurner Syndrome based on the above symptoms, we encourage you to seek medical attention for him right away.
May-Thurner Syndrome occurs when the left iliac vein is compressed by the right iliac artery, leading to restricted blood flow and vein irritation. This can be exacerbated by factors such as prolonged immobility or previous venous injury.
Common causes of May-Thurner Syndrome include:
- Compression of the left iliac vein by the right iliac artery
- Prolonged periods of immobility or sedentary lifestyle
- Previous injury or trauma to the pelvic area
- Blood clotting disorders or previous deep vein thrombosis (DVT)
Common factors that may increase your risk of developing May-Thurner Syndrome include:
- Long periods of sitting or bed rest, which can exacerbate venous compression and blood flow issues
- History of deep vein thrombosis (DVT)
- Anatomical variations that predispose individuals to the condition
At Pedes Orange County, our vascular doctors use a combination of advanced imaging techniques to accurately diagnose pelvic venous disease including May-Thurner Syndrome in our patients. These
imaging techniques include:
- Pelvic or abdominal ultrasound
- Pelvic or abdominal CT and MRI scans
Pelvic venography using X-ray imaging
We provide comprehensive treatment for May-Thurner Syndrome, utilizing advanced techniques such as angioplasty and stenting to alleviate vein compression and restore normal blood flow. In cases where
deep vein thrombosis is present, we may also employ IVC filter placement to prevent blood clots from traveling to the lungs. Our approach ensures that patients receive thorough and effective care tailored to their specific needs.
How is Pelvic Congestion Syndrome Diagnosed?
Abdominal and pelvic ultrasounds help visualize backflow in ovarian veins. But it doesn’t provide enough information, and therefore, CTs and MRIs may be used to take further images. CTS and MRIs help evaluate the pelvis
In some situations, ultrasound alone may not provide all the necessary information, and your physician may want to obtain additional imaging. For example, CT and MRI are used to take detailed pictures.

When Should I Contact My Doctor?
Some women have enlarged veins with no symptoms; others have enlarged veins that cause pains and aches. In most cases, these don’t require a medical emergency. The symptoms should reduce as you head into menopause. However, in case of chronic, unbearable pain, nothing is stopping you from seeking medical help. In fact, see your healthcare giver right away for help.
To get the most out of the consultation, here’s what to do:
- Know the purpose of the visit and what you want to get from it
- Before visiting the doctor, put down questions you need them to answer.
- Bring company along to help ask questions and note down points from the doctor.
- Please write down the name of the diagnosis, its tests, and treatment options explained by the doctor. Also, take notes of any new instructions during each visit.
- Know the reasons for new medication prescriptions, their benefits, and their risks.
- Inquire whether it’s possible to treat your condition another way
- Know why and what the results of a test procedure mean
- Ask what will happen if you don’t undergo testing or take medication.
- Ask whether a follow-up appointment is available and note down the visit’s time, date, and reason.
- Ask the doctor for their contacts in case you need a further chat.
How is Pelvic Congestion Syndrome Diagnosed?
What are the treatment options for pelvic venous congestion (PVCs)? Available treatment options for PVCs include pain-relieving progestin hormone drugs, ovarian function-blocking Gonadotropin-releasing hormones, pelvic venous embolization…

Vein Disease Specialist in Irvine, CA
If you’re experiencing chronic pelvic pain and haven’t found relief, you may be suffering from pelvic venous disease. Reach out to Pedes Orange County in Irvine, CA, at (949) 387-4724 to schedule a consultation with one of our experienced vascular specialists or contact us online for more information about our pelvic venous congestion syndrome and May-Thurner Syndrome treatments. We look forward to helping you return to a pain-free life.
Contact Us Today
Make an Appointment


Our Vascular Disease Physicians
The physicians at Pedes Orange County devote their lives to saving limbs and minimizing pain. Our conveniently located, state-of-the-art facility is designed for your comfort and utilizes cutting-edge technology to provide minimally invasive treatments. Our vascular specialists are board-certified and some of the best in Southern California. Personable staff members make every visit a positive experience, with short wait times and an efficient, streamlined process that ensures you leave feeling educated and confident that you are in good hands.

J. Joseph Hewett, M.D.
Vascular Specialist

Neil K. Goldstein, M.D.
Vascular Specialist

Derrick Tran, MD
Vascular Specialist

Mohammad Jaber, M.D.
Vascular Specialist
What to Expect from Your Visit to Pedes

Ultrasound
Advanced ultrasound-guided examination techniques will be used to visualize the veins, arteries, or both, in your legs. This is often used in the diagnostic process to detect the presence and extent of disease.

Consult
Once we review the results of your diagnostic tests, our physicians will collaborate with you to develop a personalized treatment plan, ensuring the best course of treatment for your specific condition.

Treatment
Your treatment plan will be personalized to you and your individual needs. At Pedes, we specialize in minimally invasive procedures and nonsurgical treatments, all of which are performed by our dedicated vascular physicians within the comfort of our state-of-the-art facility.

Follow up
We ensure our patients receive continuous care and support with regular follow-up visits. Each follow-up visit is scheduled at the time of your in-office appointment. Should you have a concern between appointments, we encourage you to call our office and get scheduled at any time.

Vascular Disease
Pre-register for your visit to Pedes Orange County by downloading our patient forms.






