Peripheral Arterial Disease (PAD)
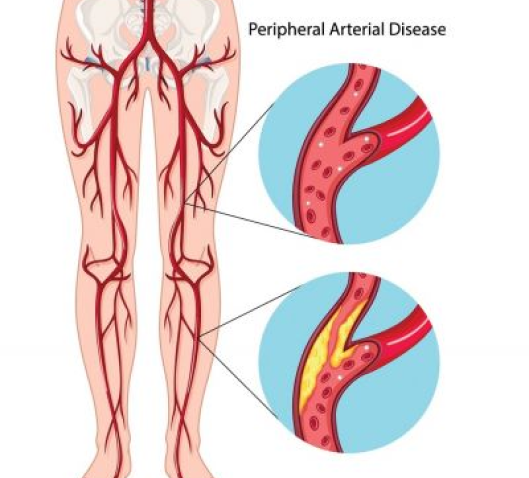
Peripheral artery disease is a subset disease of vascular disease
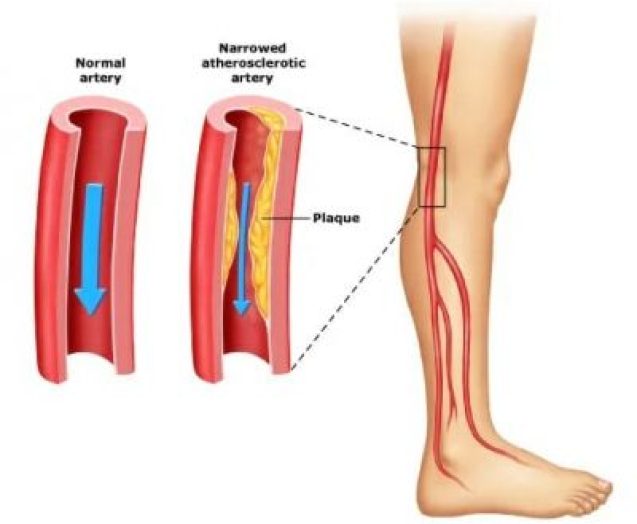
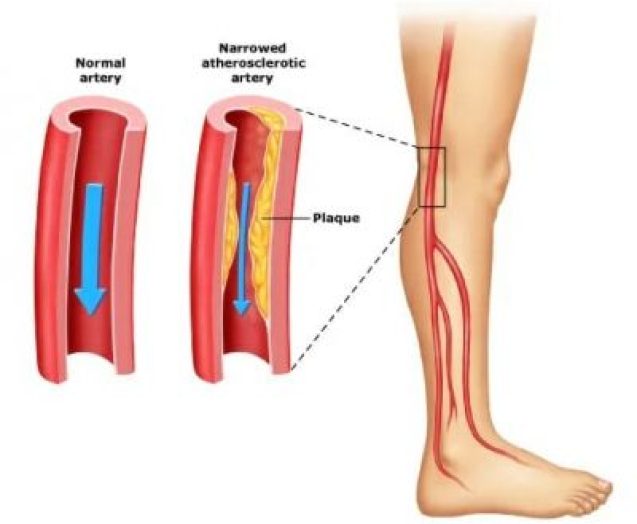
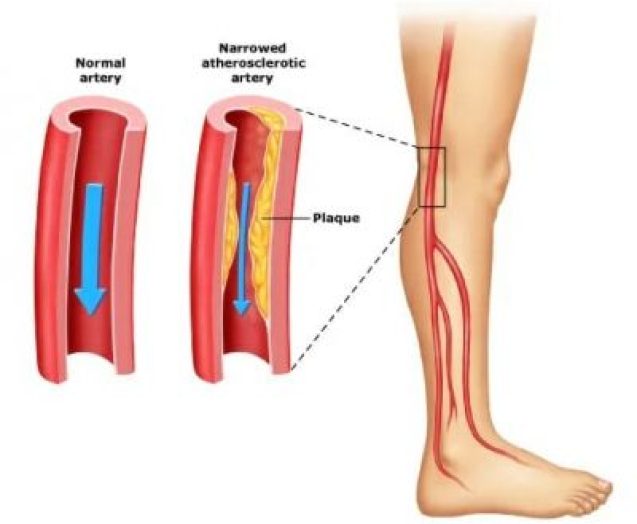
Also referred to as peripheral arterial disease (PAD), which develops when excessive plaque buildup on the artery walls, causing narrowing of the arteries. The arteries deliver oxygen-rich blood from the heart to other parts of the body. When plaque builds up, it usually restricts the flow of blood, oxygen, and glucose. The obstruction causes pain in the leg as the muscles and tissues are starved for oxygen and other nutrients from the blood. While the pain usually occurs in your legs primarily, it can also be felt in other parts of the body, including your arms, stomach, hip, head, and kidneys.
What is Peripheral Arterial Disease?
Peripheral arterial disease (PAD) develops when excessive plaque builds up on the artery walls, causing narrowing of the arteries. The arteries deliver oxygen-rich blood from the heart to other parts of the body. When plaque builds up, it usually restricts the flow of blood, oxygen, and glucose.
This obstruction causes leg pain, as the muscles and tissues are starved for oxygen and other nutrients from the blood. While the pain typically occurs in the legs, it can also be felt in the arms, stomach, hips, head, and kidneys.
PAD often manifests through claudication, a common condition that causes cramping in the legs and buttocks. This is due to the buildup of fat and cholesterol on the artery walls leading to ischemia, a condition where the demand for oxygen exceeds the supply.
Approximately half of all individuals with PAD experience occasional claudication. The discomfort caused by claudication may range from mild discomfort to debilitating pain, and may also be accompanied by the following common symptoms:
• Experiences of leg weakness, numbness, or cold feet.
• Foot or toe pain during rest.
• Non-healing wounds developing on legs, feet or toes.
• Slow toenail growth
• Changes in foot color.
• Weak pulse in the lower extremities.
• Developing shiny skin on legs.
• Pain in arms while performing manual tasks.
• Erectile dysfunction in men.
PAD is primarily caused by atherosclerosis, where fatty deposits build up in the arteries, reducing blood flow to the limbs. The lack of blood flow to the limbs is what classifies PAD. Less common causes of PAD include inflammation of the blood vessels, injury to the limbs, exposure to radiation, and general changes to the muscles or ligaments in the limbs.
PAD is significantly influenced by several risk factors, including smoking, diabetes, hypertension, and high cholesterol. Individuals with a family history of vascular diseases are also at heightened risk. Inactivity and obesity further contribute to the development of PAD, making lifestyle modifications crucial for prevention. Early identification and management of these risk factors are essential to mitigate the progression of PAD and associated complications.
Diagnosing Peripheral Arterial Disease (PAD)
At Pedes Orange County, we have highly trained physicians who offer a comprehensive diagnosis to develop customized treatments of Peripheral artery disease (PAD). We understand that no two patients’ conditions are similar. Our full-service vascular lab provides state-of-the-art testing to ensure that our physicians address each patient’s case quickly and accurately. Our doctors and nurses also have broad experience in this field and use advanced tools to achieve limb-saving results even for challenging, impaired patients.
Our PAD diagnostic process involves the following:
Our experienced doctor will conduct a comprehensive physical examination to help diagnose PAD. Our provider may ask you questions about your medical history, including specific conditions like diabetes, heart disease, and kidney disease; lifestyle habits such as smoking; and symptoms like leg pain or cramping. Following these discussions, we will assess your physical health, focusing on your legs, checking for weak pulses, poor blood flow, sores, swelling, and skin discoloration.
Ankle-brachial index (ABI tests) help diagnose PAD. This test usually compares the blood pressure in your arm with the blood pressure in your ankle. Our doctors usually use a blood pressure cuff in conjunction with an ultrasound device to carry out this test. Sometimes, our physician may request you walk on a treadmill and will take readings before and immediately after the exercise. ABI tests will help our doctors capture the severity of your narrowed arteries.
Our doctors use ultrasound-guided procedures to identify blockages or concerns within veins or arteries. This non-invasive technique uses sound waves to visualize the artery and measure blood volume, ensuring patient comfort. Following the procedure, our doctors will suggest the most effective treatment to enhance blood flow to the feet and legs, mitigating leg pain, aiding in healing wounds, and improving the limb’s mobility.
Two main ultrasound methods used are:
• Doppler ultrasound for locating areas with blockages or reduced blood flow.
• Segmental Doppler pressure testing to examine the legs for obstructed or narrowed arteries.
Angiography is a minimally invasive technique that helps our doctors visualize and diagnose blockages inside veins and arteries. In this procedure, our physician will insert a thin tube into your affected area, which will introduce a special dye that enables blood vessels to appear on an X-ray. As the dye is
introduced to the arteries and veins, fluoroscopy imaging captures the detailed images to see the extent of blockages in the arteries.
Our doctors may take a sample of your blood to measure cholesterol and triglyceride levels. Blood samples are also used to check for diabetes.
MRA tests are conducted to examine the structure of the arteries in the leg. However, your doctor will speak to you before using the procedure to ensure it best suits your needs. Magnetic resonance angiography is not recommended for people with metal implants in their bodies.
Patient Story
Treatments for Peripheral Arterial Disease (PAD)
Pedes Orange County provides comprehensive treatment for peripheral arterial disease, utilizing advanced procedures such as atherectomy, stenting, and angioplasty. Our experienced medical team ensures each patient receives tailored care aimed at restoring optimal vascular health and improving quality of life.
Are You at Risk for Peripheral Arterial Disease (PAD)?
See if you are at risk for peripheral arterial disease by taking this simple, 7-question quiz.
Artery Disease Doctor Near Me in Irvine, CA
Don’t wait to start treatment for your peripheral arterial disease. Instead, call the dedicated vascular physicians at Pedes Orange County in Irvine, CA. Call (949) 387-4724 today to make an appointment or contact our friendly staff online at your convenience. We look forward to helping you achieve optimal health.
Contact Us Today


Our Vascular Disease Physicians
The physicians at Pedes Orange County devote their lives to saving limbs and minimizing pain. Our conveniently located, state-of-the-art facility is designed for your comfort and utilizes cutting-edge technology to provide minimally invasive treatments. Our vascular specialists are board-certified and some of the best in Southern California. Personable staff members make every visit a positive experience, with short wait times and an efficient, streamlined process that ensures you leave feeling educated and confident that you are in good hands.

J. Joseph Hewett, M.D.
Vascular Specialist

Neil K. Goldstein, M.D.
Vascular Specialist

Derrick Tran, MD
Vascular Specialist

Mohammad Jaber, M.D.
Vascular Specialist
Why Choose Pedes Orange County
Pedes Orange County is dedicated to providing personalized arterial treatments aimed at reducing pain, promoting speedy healing and, most importantly, preventing amputation. Our treatments are designed to enhance the quality of our patients’ lives by rapidly halting disease progression.
Our physicians and vascular specialists prioritize your needs, leveraging our vast experience to offer precise treatments and lifestyle advice to prevent recurrence. Our patient care extends beyond the procedure, with scheduled follow-ups to track recovery and to deal with any concerns. Schedule an appointment today and experience our commitment to delivering the best results.
What to Expect from Your Visit to Pedes

Ultrasound
Advanced ultrasound-guided examination techniques will be used to visualize the veins, arteries, or both, in your legs. This is often used in the diagnostic process to detect the presence and extent of disease.

Consult
Once we review the results of your diagnostic tests, our physicians will collaborate with you to develop a personalized treatment plan, ensuring the best course of treatment for your specific condition.

Treatment
Your treatment plan will be personalized to you and your individual needs. At Pedes, we specialize in minimally invasive procedures and nonsurgical treatments, all of which are performed by our dedicated vascular physicians within the comfort of our state-of-the-art facility.

Follow up
We ensure our patients receive continuous care and support with regular follow-up visits. Each follow-up visit is scheduled at the time of your in-office appointment. Should you have a concern between
appointments, we encourage you to call our office and get scheduled at any time.








